Journey of Magnet Excellence
For nearly six decades, Gracie Square Hospital has been a mainstay of the Upper East Side, providing the highest quality and most compassionate care to adults 18 years and older with behavioral health needs who can benefit from inpatient hospitalization. Gracie Square Hospital offers individuals a warm and welcoming environment in which to receive state-of-the-art treatment to facilitate a healthy recovery.
Gracie Square Hospital Executive Director & Chief Nursing Officer
Dear Colleagues,

We Did It!! We are now a Magnet® designated organization! 2022 was a truly amazing year! We have so much to be proud of and acknowledge. Despite the unprecedented challenges over the past several years, we accomplished extraordinary goals as one team. Throughout 2022 we worked together to achieve a successful Magnet site visit. So much time and planning went into the preparation for this visit, and the teamwork paid off tremendously. On December 14, 2022, we received a call from the American Nurse Credentialing Center’s (ANCC) Commission on Magnet® who made the announcement that Gracie Square Hospital achieved Magnet® designation. Everyone, whether you met with the appraisers or stayed on the unit caring for patients, was exceptional. The appraisers were so impressed with the nurses, support staff, Board of Trustees, and our community partners. Our site visit was described as “magical” - there was so much tangible energy and enthusiasm! Thank you to everyone involved in this extraordinary recognition for the work you do every day.
This significant accomplishment sets the stage for what’s ahead in 2023. We are excited to finalize our Planetree Gold re-application, due in March 2023. Thank you to all who have worked so hard toward achieving this important goal. Our quality clinical indicators continue to be met and our employee engagement scores, released in 2022, were fantastic. The GSH mean in 2019 was 3.68 and improved to 4.01 in 2022. In addition, employees reported a significant increase in all 3 safety culture scores from 2021 to 2022. Thanks again to all the employees who completed this survey. Managers for each department will be facilitating employee engagement goals and tactics for 2023 based on your input and ideas.
In addition to continuing to celebrate our Magnet Designation and expected Planetree recognition, we plan are revamping our professional governance committee structure in 2023. We kicked off the improvements in January 2023, making the second Tuesday of each month designated as scheduled time for collaboration and innovation initiatives and meetings. Also in January 2023, we began the GSH Nursing Clinical Ladder as a professional development and recognition program for increasing nurse satisfaction, retention, and recognition opportunities.
On the facilities side, construction work in day rooms will be completed in 2023 to meet external safety requirements. We will also be completing significant work in the employee locker rooms. This work is scheduled to begin in early 2023. Dr. Wilner and I will be seeking your input into the design of the renovated locker rooms.
Thank you for contributions you make to patients, each other, and the communities. We continue to highlight Gracie Square Hospital and the wonderful work done by all of you. Please be sure to look for GSH on LinkedIn, Instagram, and other social media outlets.
Sincerely,
Timothy P. McGarvey MSN, LMSW, RN, NEA-BC
Executive Director & Chief Nursing Officer
Gracie Square Nursing Department: Our Mission & Vision
The foundation to our journey of nursing excellence is our commitment to our patients and communities as expressed in our mission and vision statements. Through our Professional Governance Model, our nurses own their professional practice, allowing each individual to perform to the top of their professional license.
Mission
To serve our communities by providing world-class person and family centered care in an empowering and innovative professional nursing practice environment.
Vision
To be the world leader in nursing.
- Proactive
- Quality, Safety, and Outcomes
- Research
- Education
- Service Excellence
The Roadmap – Our Strategic Plan
This is a “living” document that is the basis of the work we do to promote professional development, patient safety and quality care, an improved work environment, utilization of technology to support nurses in the day to day functions, and patient engagement in achieving health and well-being. The Strategic Plan consists of the following major domains: professional development and education, quality and patient safety, advancing care, operational excellence, technology innovation, nursing engagement, and patient-family experience.
| Themes (Areas of Focus) | What we want to accomplish |
|---|---|
| Professional Development and Education (PDE) |
|
| Quality and Safety (QS) |
|
| Advancing Care/Professional Practice/Shared Governance (AC) |
|
| Operational Excellence (OE) |
|
| Technology Innovation (TI) |
|
| Patient and Nurse Experience (PSX) |
|
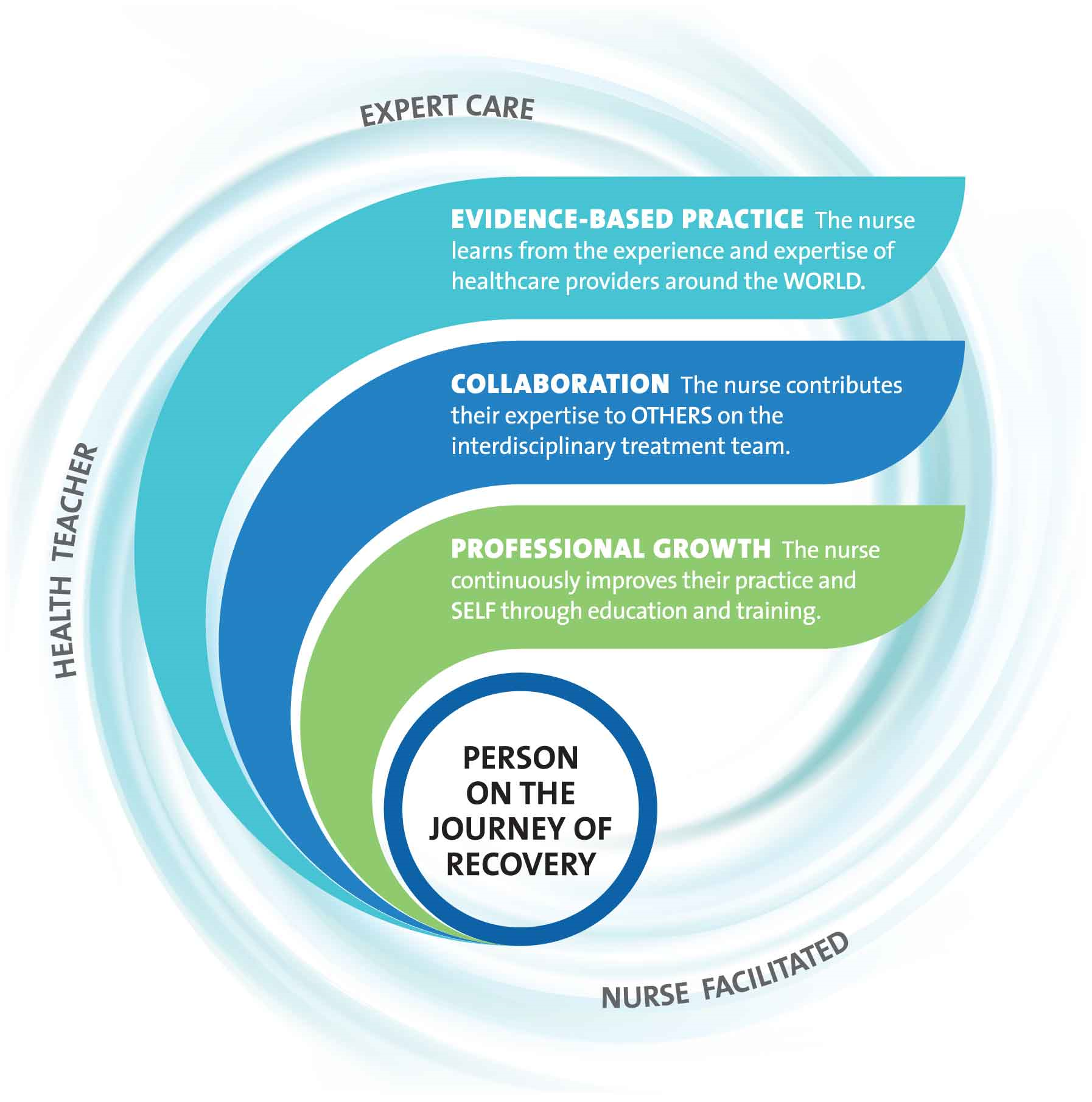
Our Professional Practice Model
2024 Measures of Distinction
40%
National Board Certification Rate
94%
Percent of RNs with BSN and Higher Degrees
6
Newly Obtained National Board Certification
10
Formal Degrees Conferred
1
Nursing Research Studies Completed
3
Nursing Research Studies in Progress
0
Professional Publication(s)
0
Podium Presentation(s)
1
Poster Presentation(s)
2024 Contributions of Nurses
Organization Prioritizes Workplace Safety with Personal Response Devices
During a 2024 interprofessional Violence Reduction Committee meeting, clinical nurses communicated concerns about escalating workplace violence. Although the units had stationary wall-access panic buttons, the nursing staff experienced challenges associated with leaving the area to locate the closest panic button at the time of the event. The suggestion was made to implement a personal alarm system, which would equip each employee with a wearable safety response badge. Nursing and interprofessional leaders and clinical teams promoted the benefits of personal alarms, including the potential to not only reduce workplace violence by improving emergency response efficiency but also reduce delays in patient care.
Nurse leaders used the input from the clinical nurses to influence change when they implemented the personal employee response system. The system allows team members to quickly and discreetly activate a psychiatric emergency by pressing a wearable badge that sends alerts to all employees’ mobile devices indicating the employee’s name. The system also generates a map tracking the employee’s location in real time, allowing staff to identify the location to provide prompt emergency support.
Outcome
Fifty-one percent of the nursing staff participated in the pre- and post-survey to assess employee attitudes towards workplace safety and emergency response efficiency. Prior to the implementation of the employee response system, 75 percent of participants responded that they felt the organization was actively working to improve their safety. Post-implementation, 88 percent of the participants reported improved perceptions of their safety in the workplace. When asked if they felt confident that they would receive help when unsafe at work, 78 percent responded favorably prior to implementation. However, post-implementation, 96 percent of nursing staff reported confidence in receiving help. Overall, 80 percent of participants reported feeling safer at work with the change and improvements in psychiatric emergency responses.
Mentoring Nurse Researchers: Strengthening Professional Development for Research Team Members
Gracie Square Hospital team members are committed to supporting clinical nurses’ professional development, including nurses’ participation in mentorship, research, and professional organizations. Proudly designated an LGBTQ+ Healthcare Equality Leader by the Healthcare Equality Index (HEI) of the Human Rights Campaign, Gracie Square conducted nursing research examining healthcare personnel’s attitudes on delivering culturally sensitive care to LGBTQ+ patients. During the Nursing Research and Evidence-Based Practice Committee meeting, two of the study’s principal investigators Kasey Jackman, PhD, RN, PMHNP-BC, FAAN, nurse scientist, NewYork-Presbyterian, and Ray Gannon, PhD, MSN, AGPCNP-BC, nurse scientist and Director, Research Fellowship, NewYork-Presbyterian, solicited clinical nurse volunteers to join the research team. Engaged committee member Rasaan Ogilvie, BSN, RN, a new psychiatric-mental health clinical nurse with the Young Adult-College Track Program, joined the research team and was mentored by Dr. Jackman and Dr. Gannon extensively throughout 2024 on conducting and presenting nursing research.
Outcome
Thanks to Dr. Jackman’s and Dr. Gannon’s mentorship, as well as the organization’s support, Mr. Ogilvie confidently took advantage of professional development opportunities to present the group’s research in multiple forums, including NewYork-Presbyterian Grand Rounds, NewYork-Presbyterian’s first annual Psychiatric-Mental Health Nursing Summit, and the Gay and Lesbian Medical Association’s 2024 Annual Conference on LGBTQ+ Health held in North Carolina. Mr. Ogilvie is working on a manuscript for publication and was accepted as a presenter for the LGBT Health Workforce Conference in New York City.
Falls Prevention Strategies Improve Patient Safety for Older Adults
The Older Adults and Asian Program (OAAP) nursing team prioritizes falls prevention as a critical unit goal to demonstrate excellence in patient care and patient safety. As members of the OAAP Unit Practice Council, clinical nurses continuously evaluate falls data and prevention strategies to identify opportunities for improvement. Throughout 2024, the OAAP Unit Practice Council implemented a bundle of strategies to reduce falls, including Bingo Friday, an engaging weekly nurse-led patient education group structured around the game Bingo; walker pouches that attach to geriatric patients’ walkers allowing them to carry personal items while safely ambulating the unit; and patient bed alarms to swiftly alert others when patients attempt to get out of bed unassisted. The OAAP Unit Practice Council members also actively promoted collaboration with physical therapy, encouraging clinical nurses to initiate physical therapy consults more readily for patients identified as high risk for falls and to support those patients’ participation in biweekly physical therapy sessions.
Outcome
As a result of the OAAP Unit Practice Council’s comprehensive bundle of targeted falls prevention strategies, the unit’s total unassisted fall events decreased 14 percent in 2024 when compared to the previous year.
A New Evidence-Based Practice to Improve Patient Safety
Aggressive behaviors are associated with various psychiatric disorders and have a significant negative impact on patients, healthcare workers, and the practice environment. Escalating behaviors and aggressive actions can have detrimental effects to patients exhibiting, witnessing, or victimized by the behavior, and staff attempting to therapeutically manage the behavior, often resulting in the use of restraints to ensure a patient’s safety to self and/or others. Gracie Square implemented the Aggression Prevention Protocol, an evidence-based strategy for proactive violence prevention for all patients assessed to be high risk for aggression as determined by the evidence-based Dynamic Appraisal of Situational Aggression (DASA) risk assessment tool. Similar to a clinical decision tool or algorithm, the Aggression Prevention Protocol suggests evidence-based interventions for violence prevention specific to a patient’s risk level. In conjunction with DASA, the Aggression Prevention Protocol has been associated with reduced aggression as well as the use of restrictive interventions such as restraints.
Outcome
Following the clinical nurses’ implementation of the Aggression Prevention Protocol, an effective evidence-based practice, the restraint rate decreased by 36.8 percent and the seclusion rate decreased by 14.78 percent.
Implementing Ketamine Infusion Therapy for Treatment-Resistant Depression
Ketamine infusion therapy has been shown to rapidly reduce suicidal ideation and symptoms of depression, particularly in patients with treatment-resistant major depressive disorder. During 2024, a collaborative interprofessional team, inclusive of providers, nurses, leaders, and pharmacists, planned for implementation of ketamine infusion therapy. They designed a space for treatment, ensured the procurement of medications and supplies, and finalized interprofessional clinical workflows and policies. Nursing education was a major consideration as peripheral intravenous (PIV) access and line maintenance were not existing psychiatric-mental health nursing competencies. The nurse educators worked closely with a core group of clinical nurses to develop comprehensive targeted PIV and intravenous pump education to address the competency gap.
Outcome
In November 2024, providers and nurses initiated ketamine therapy. Patient responses to treatment were measured using the Montgomery-Asberg Depression Rating Scale, which demonstrated a statistically significant improvement. On average, patients receiving ketamine infusion therapy reported greater than 50 percent reduction in depressive symptoms one week post-treatment. Among patients receiving ketamine infusion therapy, the clinical team noted a mean length of stay of 9.60 days, much lower than the organization’s overall mean length of stay of 16.97 days.


